Connect With Us
Blog

Facts About Plantar Fasciitis and Its Symptoms
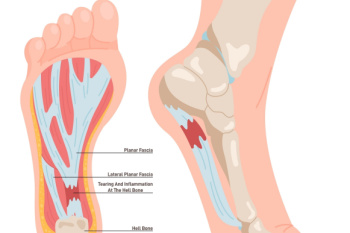
Plantar fasciitis is a common cause of heel pain, resulting from inflammation of the plantar fascia, which is the thick band of tissue that runs along the bottom of the foot and connects the heel bone to the toes. The condition typically causes a sharp, stabbing pain in the heel, particularly noticeable with the first steps in the morning or after periods of inactivity. Risk factors include prolonged standing, high-impact activities, obesity, and wearing unsupportive shoes. The pain usually lessens with movement but can return after long periods of standing or sitting. Treatment often involves stretching exercises, wearing proper footwear, and rest to reduce inflammation. In severe cases, orthotics or injections may be necessary. Plantar fasciitis can cause severe pain and can hinder completing daily activities. If you have heel pain, it is strongly suggested that you are under the care of a podiatrist who can accurately diagnose and treat plantar fasciitis.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Royall from Mountain View Foot & Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
What are Pressure Ulcers on the Feet and Ankles?
 Pressure ulcers on the feet and ankles, also known as pressure sores or bedsores, are injuries to the skin and underlying tissue resulting from prolonged pressure. These ulcers are common in individuals with limited mobility, and can often affect the feet. Intrinsic factors, such as poor nutrition, age, and medical conditions like diabetes, affect the body's ability to heal and withstand pressure. Extrinsic factors involve external forces like friction and prolonged pressure from staying in one position. Symptoms include redness, pain, and open sores, which can progress to deep wounds exposing muscle and bone. Pressure ulcers occur due to reduced blood flow to the affected area, leading to tissue damage. Prevention includes regularly changing positions, using supportive devices, maintaining good nutrition, and keeping the skin clean and dry. Treatment involves relieving pressure, cleaning wounds, and using dressings or medications to promote healing. Advanced cases might require surgical intervention. If you are suffering from a pressure ulcer on your feet or ankles, it is suggested that you schedule an appointment with a podiatrist as soon as possible for care.
Pressure ulcers on the feet and ankles, also known as pressure sores or bedsores, are injuries to the skin and underlying tissue resulting from prolonged pressure. These ulcers are common in individuals with limited mobility, and can often affect the feet. Intrinsic factors, such as poor nutrition, age, and medical conditions like diabetes, affect the body's ability to heal and withstand pressure. Extrinsic factors involve external forces like friction and prolonged pressure from staying in one position. Symptoms include redness, pain, and open sores, which can progress to deep wounds exposing muscle and bone. Pressure ulcers occur due to reduced blood flow to the affected area, leading to tissue damage. Prevention includes regularly changing positions, using supportive devices, maintaining good nutrition, and keeping the skin clean and dry. Treatment involves relieving pressure, cleaning wounds, and using dressings or medications to promote healing. Advanced cases might require surgical intervention. If you are suffering from a pressure ulcer on your feet or ankles, it is suggested that you schedule an appointment with a podiatrist as soon as possible for care.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Royall from Mountain View Foot & Ankle Clinic. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Symptoms of Poor Circulation in the Feet

Poor circulation in the feet manifests through various symptoms, possibly indicating underlying health issues. Cold feet are a common sign, often accompanied by tingling or numbness due to reduced blood flow. Swelling can occur as fluid accumulates, causing discomfort and making it difficult to wear shoes. Pain and a sense of heaviness in the feet may also develop, impacting mobility and daily activities. Discoloration, such as a bluish or pale hue, suggests insufficient oxygen supply. Additionally, poor circulation can lead to itchy rashes or dry skin, exacerbating discomfort. Improving circulation through lifestyle changes, medical treatments, and proper foot care may alleviate these issues. If you have any of the above symptoms, it is suggested that you consult a podiatrist who can diagnose and treat poor circulation.
Poor circulation is a serious condition and needs immediate medical attention. If you have any concerns with poor circulation in your feet contact Dr. Royall of Mountain View Foot & Ankle Clinic. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Poor blood circulation in the feet and legs is can be caused by peripheral artery disease (PAD), which is the result of a buildup of plaque in the arteries.
Plaque buildup or atherosclerosis results from excess calcium and cholesterol in the bloodstream. This can restrict the amount of blood which can flow through the arteries. Poor blood circulation in the feet and legs are sometimes caused by inflammation in the blood vessels, known as vasculitis.
Causes
Lack of oxygen and oxygen from poor blood circulation restricts muscle growth and development. It can also cause:
- Muscle pain, stiffness, or weakness
- Numbness or cramping in the legs
- Skin discoloration
- Slower nail & hair growth
- Erectile dysfunction
Those who have diabetes or smoke are at greatest risk for poor circulation, as are those who are over 50. If you have poor circulation in the feet and legs it may be caused by PAD and is important to make changes to your lifestyle in order to reduce risk of getting a heart attack or stroke. Exercise and maintaining a healthy lifestyle will dramatically improve conditions.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment of Poor Blood Circulation in the Feet
Poor blood circulation in the feet and legs is often caused by peripheral artery disease (PAD), which is usually the result of a buildup of plaque in the arteries. Plaque buildup, or atherosclerosis, can be the result of excess calcium and cholesterol in the bloodstream. This restricts how much blood can flow through arteries. Reduced blood flow to a certain area of the body severely limits the amount of oxygen and nutrients that part of the body receives. This leads to degeneration in the muscles and other tissues. Sometimes, poor blood circulation in the feet and legs can be caused by other conditions, such as the damaging or inflammation of blood vessels, known as vasculitis.
The lack of oxygen and nutrients caused by poor blood circulation can restrict muscle growth and development, as well as cause muscle pain and cramps, weakness, and stiffness. Other common symptoms include numbness in the legs and feet, skin discoloration in the affected limbs, slower nail and hair growth, and erectile dysfunction in men. In more severe cases of PAD, pain can be present even when a person isn't exercising, and may range from mildly uncomfortable to completely debilitating.
Poor blood circulation in the feet and legs is more common in those who are overweight or obese, have diabetes, high blood pressure, high cholesterol, who smoke, or who have a family history of PAD or related conditions such as a heart attack, stroke, etc. Diabetes and smoking place a person at greatest risk for developing poor blood circulation, although advanced age, over 50, can also increase risk.
If you are experiencing poor blood circulation in the feet and legs caused by PAD, it is important to make changes to your lifestyle in order to reduce your risk of experiencing a heart attack or stroke caused by this condition. If you smoke, quit completely. This will increase the amount of oxygen in your bloodstream. Exercising and reducing the saturated fats in your diet. Saturated fats come from fatty meats, fried foods, whole milk, etc., can make a difference in improving blood circulation in feet. It is also important to avoid developing influenza and to carefully control your blood sugar if you have diabetes.
Your doctor may recommend combining lifestyle changes with a prescription medication regimen to improve blood circulation. The most commonly-used medications for PAD are called statins and work by blocking the amount of enzymes in your body that produce cholesterol. They are known by the brand names Zocor, Lipitor, Crestor, and others.
Sports Foot and Ankle Injuries Common in Children
 Children's participation in sports brings numerous benefits, but it also comes with the risk of acute and overuse injuries to their feet and ankles. Physiological and physical differences between children and adults make kids particularly vulnerable to these injuries. Children's bones are still developing, making them more prone to fractures, growth plate injuries, and tendon strains. Additionally, their muscles and ligaments are less developed and may not provide adequate support during physical activity, increasing the risk of sprains and overuse injuries. Common foot and ankle injuries among kids involved in sports include ankle sprains, Sever's disease, stress fractures, and Achilles tendonitis. These injuries can significantly impact a child's participation in sports and overall quality of life if not properly addressed. If your child experiences foot or ankle pain during or after sports activities, it is suggested that you consult a podiatrist for a thorough evaluation and appropriate management. Early intervention can prevent long-term complications and facilitate a safe return to sports.
Children's participation in sports brings numerous benefits, but it also comes with the risk of acute and overuse injuries to their feet and ankles. Physiological and physical differences between children and adults make kids particularly vulnerable to these injuries. Children's bones are still developing, making them more prone to fractures, growth plate injuries, and tendon strains. Additionally, their muscles and ligaments are less developed and may not provide adequate support during physical activity, increasing the risk of sprains and overuse injuries. Common foot and ankle injuries among kids involved in sports include ankle sprains, Sever's disease, stress fractures, and Achilles tendonitis. These injuries can significantly impact a child's participation in sports and overall quality of life if not properly addressed. If your child experiences foot or ankle pain during or after sports activities, it is suggested that you consult a podiatrist for a thorough evaluation and appropriate management. Early intervention can prevent long-term complications and facilitate a safe return to sports.
Sports related foot and ankle injuries require proper treatment before players can go back to their regular routines. For more information, contact Dr. Royall of Mountain View Foot & Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are a common occurrence when it comes to athletes of any sport. While many athletes dismiss the initial aches and pains, the truth is that ignoring potential foot and ankle injuries can lead to serious problems. As athletes continue to place pressure and strain the area further, a mild injury can turn into something as serious as a rupture and may lead to a permanent disability. There are many factors that contribute to sports related foot and ankle injuries, which include failure to warm up properly, not providing support or wearing bad footwear. Common injuries and conditions athletes face, including:
- Plantar Fasciitis
- Plantar Fasciosis
- Achilles Tendinitis
- Achilles Tendon Rupture
- Ankle Sprains
Sports related injuries are commonly treated using the RICE method. This includes rest, applying ice to the injured area, compression and elevating the ankle. More serious sprains and injuries may require surgery, which could include arthroscopic and reconstructive surgery. Rehabilitation and therapy may also be required in order to get any recovering athlete to become fully functional again. Any unusual aches and pains an athlete sustains must be evaluated by a licensed, reputable medical professional.
If you have any questions please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sports Related Foot And Ankle Injuries
Foot and ankle injuries are common among people who participate in sports. Several factors contribute to this. They include failing to stretch or warm up properly, not wearing the proper type of shoe and not taping or providing other types of support for the ankle or foot. The most common foot and ankle injuries suffered by people involved in sports are plantar fasciitis, ankle sprains and Achilles tendon damage or ruptures. If not treated properly, they can lead to permanent disability.
Treating these injuries is relatively simple if they are identified and addressed early. Many athletes dismiss the initial aches and pains associated with injury as just soreness or tired muscles. Their first response is usually to try to work through it. This can lead to serious problems. Many minor injuries are made far more serious when athletes continue to put strain and pressure on them. That attitude can change a mild strain into a serious strain and a minor tear into a rupture. Athletes should have unusual aches and pains evaluated by a skilled medical professional.
Plantar fasciitis is a painful injury. It is inflammation of the plantar fascia, the thick band of tissue running from the heel to the base of the toes. If left untreated, it can lead to a degenerative disease called plantar fasciosis. There are several effective treatments for this ailment. Doctors often prescribe rest, massages, stretching, night splints, physical therapy, anti-inflammatory medication, corticosteroids or surgery, usually in that order. The most effective treatment for plantar fasciitis is orthotics, which offers foot support. Surgery is occasionally used as a last resort, but it comes with the risk of nerve damage and infection and often does not stop the pain.
The Achilles tendon is the largest tendon in the body. It connects the calf muscles to the heel bone. Running, jumping and walking all impact this tendon. Two common injuries to the Achilles tendon are tendonitis and a rupture of the tendon. Tendonitis is inflammation in the tendon often caused by an increase in the amount of stress placed on it. Non-surgical treatments include rest, ice or anti-inflammatory medication. A rupture (tear) of the Achilles tendon can be treated by placing the lower leg in a cast for several weeks or with surgery. Many physicians feel surgery is the better option because it lowers the risk of re-ruptures. Both methods require 4 to 6 months of rehabilitation.
Ankle sprains are the most common sports related foot and ankle injury. A sprain occurs when the ligament holding the ankle bones and joint stretches beyond its normal range. It can be treated non-surgically with a combination of rest, ice wrapped around the joint for 30 minutes immediately after injury, compression by a bandage and elevating the ankle above the heart for 48 hours. This combination is referred to as RICE. Severe ankle sprains in which the ligaments are torn may require reconstructive surgery followed by rehabilitation.
Making Sure Shoes Fit Right
 Proper shoe fitting is important for both comfort and performance, with different needs for walking and running shoes. Walking shoes prioritize support and cushioning to handle the consistent, moderate impact of walking while running shoes are designed to absorb the higher impact and repetitive strain of running. Understanding your foot type is essential in selecting the right shoe. Neutral feet maintain a balanced stride, rigid feet need more cushioning to absorb shock, and flexible feet benefit from stability features to control excessive movement. To determine your foot type, observe your arches. Low arches indicate flexible feet, high arches suggest rigid feet and neutral arches are balanced. Additionally, examining your shoe wear pattern can reveal your tread type. In the store, ensure shoes fit well without rubbing or pinching, as these issues can lead to discomfort or injury. If you are in the market for new shoes, it is suggested that you visit a podiatrist for personalized advice.
Proper shoe fitting is important for both comfort and performance, with different needs for walking and running shoes. Walking shoes prioritize support and cushioning to handle the consistent, moderate impact of walking while running shoes are designed to absorb the higher impact and repetitive strain of running. Understanding your foot type is essential in selecting the right shoe. Neutral feet maintain a balanced stride, rigid feet need more cushioning to absorb shock, and flexible feet benefit from stability features to control excessive movement. To determine your foot type, observe your arches. Low arches indicate flexible feet, high arches suggest rigid feet and neutral arches are balanced. Additionally, examining your shoe wear pattern can reveal your tread type. In the store, ensure shoes fit well without rubbing or pinching, as these issues can lead to discomfort or injury. If you are in the market for new shoes, it is suggested that you visit a podiatrist for personalized advice.
Finding a properly-fitting shoe is important in reducing injuries and preventing foot problems. For more information about treatment, contact Dr. Royall from Mountain View Foot & Ankle Clinic. Our doctor will treat your foot and ankle needs.
Proper Shoe Fitting
A common concern when it comes to foot health, having properly fitted shoes can help prevent injuries to the foot. Out feet affect our posture and gait, which in turn affects the biomechanics and overall bodily structure. With 33 joints, 26 bones, and over 100 ligaments, the potential for serious injury is much greater than one realizes. Although the feet cease growth in adulthood, they still change shape as they mature. Here are some factors to consider when it comes to investing in proper fitting shoes:
- Be sure the shoes fit correctly right away
- Ensure the ball of your foot fits comfortably in the widest portion of the shoes
- Even though they may look fashionable, improper fitting shoes can either create adverse conditions or exacerbate existing ones you may already have
- Walk along a carpeted surface to ensure the shoes comfortably fit during normal activity
Keeping in mind how shoes fit the biomechanics of your body, properly-fitting shoes are vitally important. Fortunately, it is not difficult to acquire footwear that fits correctly. Be sure to wear shoes that support the overall structure of your body. Do your feet a favor and invest in several pairs of well-fitted shoes today.
If you have any questions please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020